The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers (VA Nursing Home) Programs.
- In the ‘About’ section of this post is an overview of the issues or challenges, potential solutions, and web links. Other sections have information on relevant legislation, committees, agencies, programs in addition to information on the judiciary, nonpartisan & partisan organizations, and a wikipedia entry.
- To participate in ongoing forums, ask the post’s curators questions, and make suggestions, scroll to the ‘Discuss’ section at the bottom of each post or select the “comment” icon.
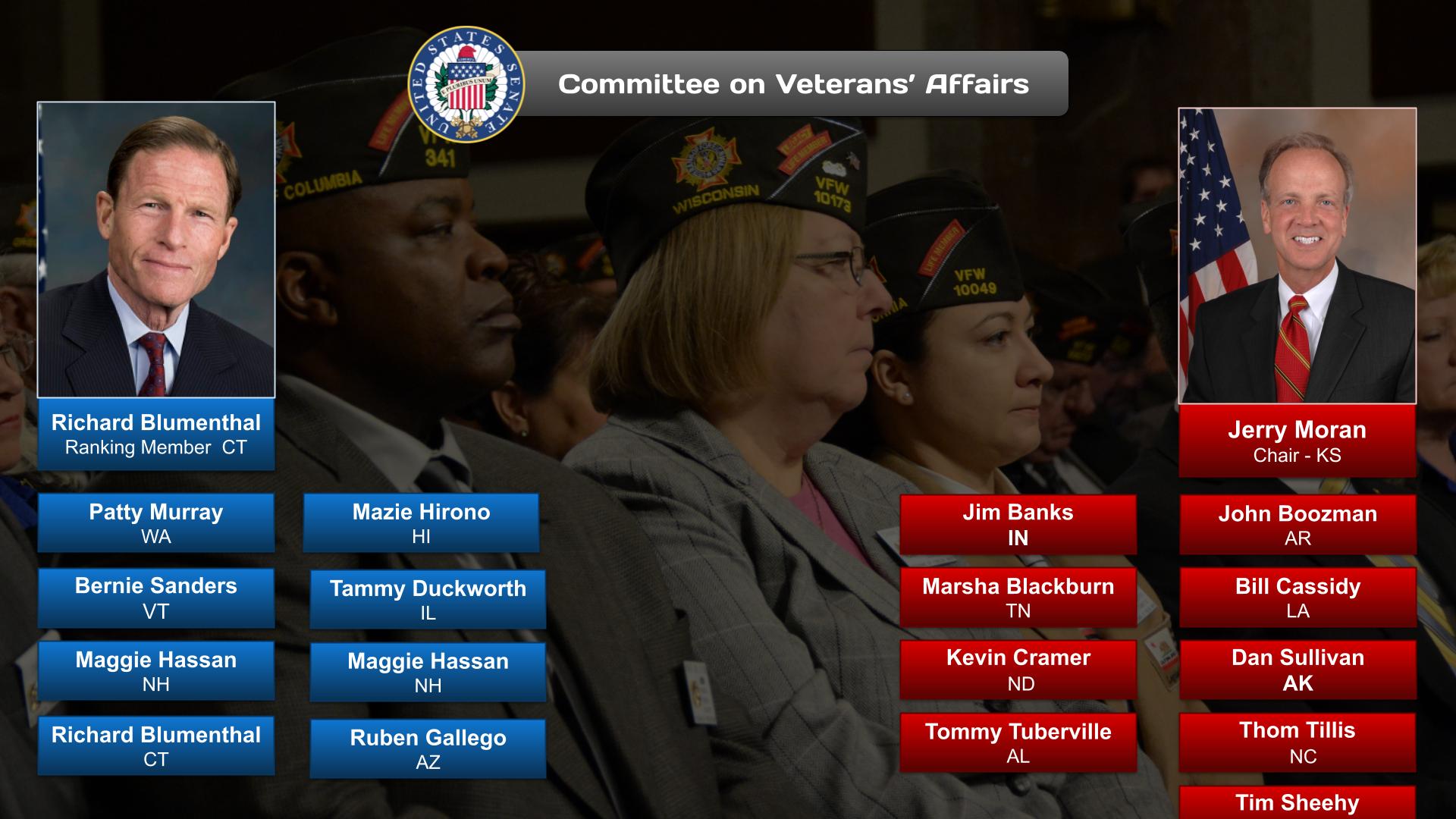
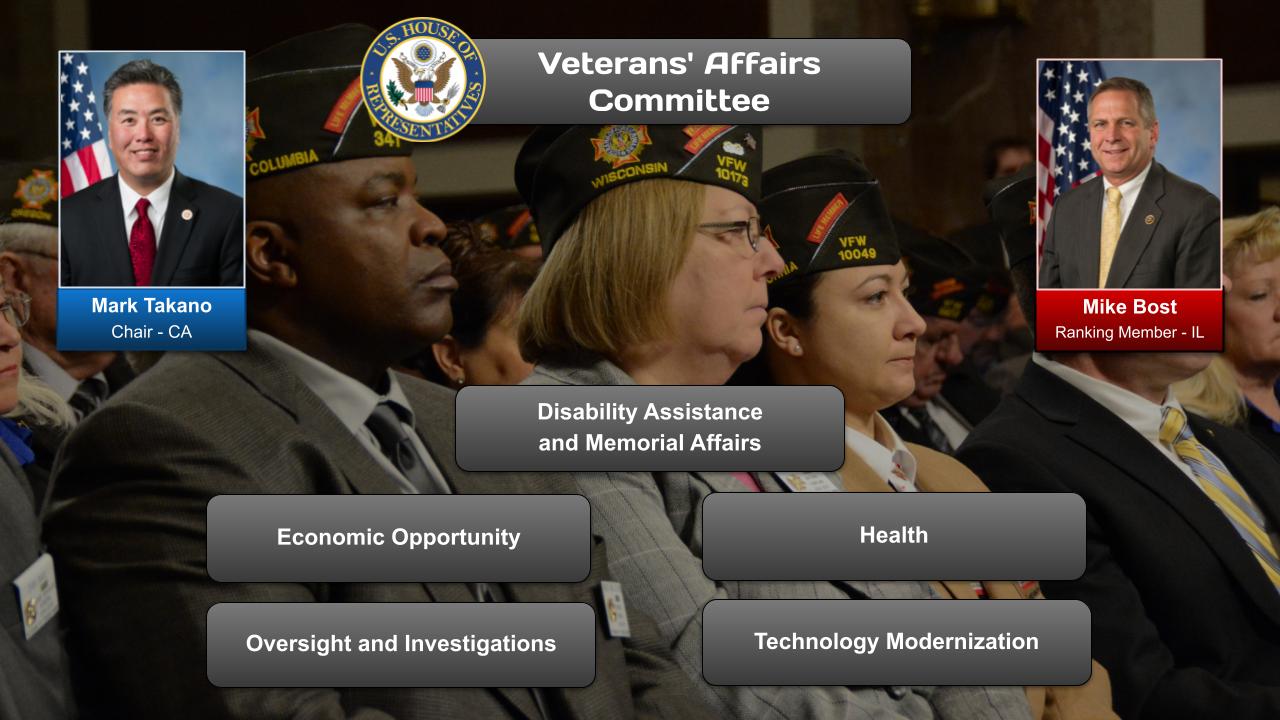
The Veterans Mental Health category has related posts on government agencies and departments and committees and their Chairs.
TEDx Talks (12:53)
https://www.youtube.com/watch?v=_ibvpvEIA3U
We always hear about how 22 veterans a day take their lives, but no one has been able to nail down the exact reasons or the path chosen for suicide to be an option. The reasons vary, the circumstances vary. As a Retired Non-Commissioned Officer of the U.S. Air Force, I can tell you firsthand how I lost my identity, and furthermore, knew it would happen. My talk will address how the military community, retired and currently serving, face an identity crisis as we exit our careers. Sean Douglas is a U.S. Air Force Veteran Retired, John Maxwell Speaker, TEDx Speaker, Top 3% Podcaster, Bestselling Author, and a Business Positioning Strategist. This talk was given at a TEDx event using the TED conference format but independently organized by a local community.
OnAir Post: Mental Health