Health promotion is a public health function that aims to improve people’s health by helping them gain control over their health and well-being. It involves a variety of strategies, including:
- Education: Improving health knowledge, attitudes, and skills
- Behavior change: Encouraging voluntary lifestyle changes to reduce risk factors
- Social and environmental interventions: Creating supportive environments, building healthy public policies, and strengthening community action
- Collaboration: Working across sectors to achieve health equity
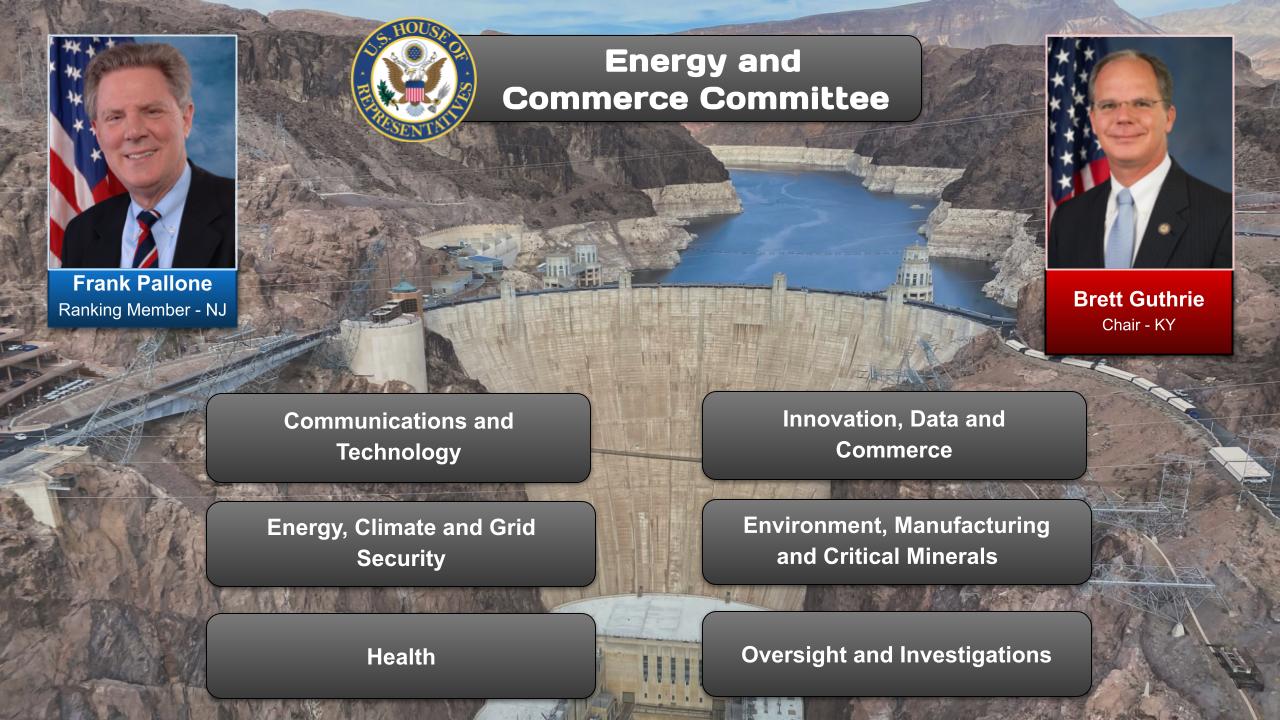
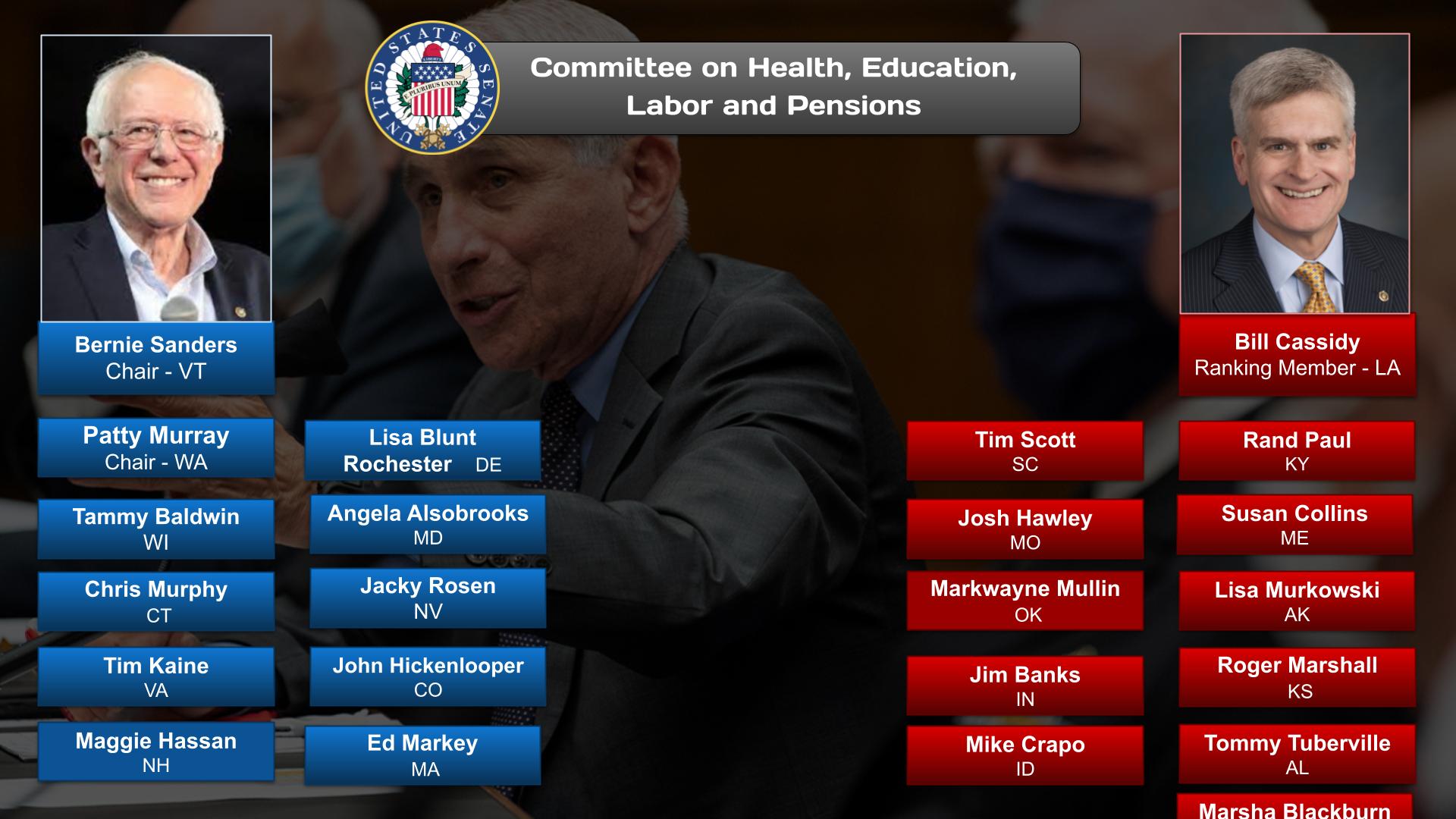
In the ‘About’ section of this post is an overview of the issues or challenges and potential solutions, and web links. Other sections have information on relevant committees, chairs, & caucuses; departments & agencies; and the judiciary, nonpartisan & partisan organizations, and a wikipedia entry.
To participate in ongoing forums, ask the post’s curators questions, and make suggestions, scroll to the ‘Discuss’ section at the bottom of each post or select the “comment” icon.
The Health Promotion category has related posts on government agencies and departments and committees and their Chairs.
PBS NOVA – 31/05/2023 (53:32)
https://www.youtube.com/watch?v=yQ6VOOd73MA&t=2s
Dive into the subconscious to see what’s really driving the decisions you make.
Official Website: https://to.pbs.org/3pUGv1s | #novapbs
Are you in control, or is your brain controlling you? Dive into the latest research on the subconscious with neuroscientist Heather Berlin. Sleepwalking, anesthesia, game theory, and more reveal surprising insights in this eye-opening journey to discover what’s really driving the decisions you make.
Chapters: 00:00 Introduction
03:22 Sleepwalking and the Brain
08:36 Anesthesia and the Brain
14:18 Results of Split Brain Surgery
22:23 Emotions and the Brain 30:01 How Does Trauma Affect the Brain?
35:39 How Much Control Do We Have of Our Brain?
45:44 Creativity and the Brain
50:17 Conclusion
OnAir Post: Health Promotion